By Hilary Pillin, UEC Strategy Advisor, AACE
Delays in being able to handover patients from ambulance crew to emergency departments in a timely manner continue to cause significant challenges for the ambulance sector. Aside from the obvious negative effects on ambulance service resources and performance, patient safety and staff wellbeing are significantly affected by protracted hospital handover delays.
We know that patients waiting over an hour outside ED are likely to incur harm in many respects. While we see a bumpy trend line over the last couple of years (with the trend since December 2024 being downward) the overall trajectory for handover delays remains upwards. This is frustrating considering the significant efforts being made by ambulance trusts, acute partners and ICBs across the country to try and counter these long waits.
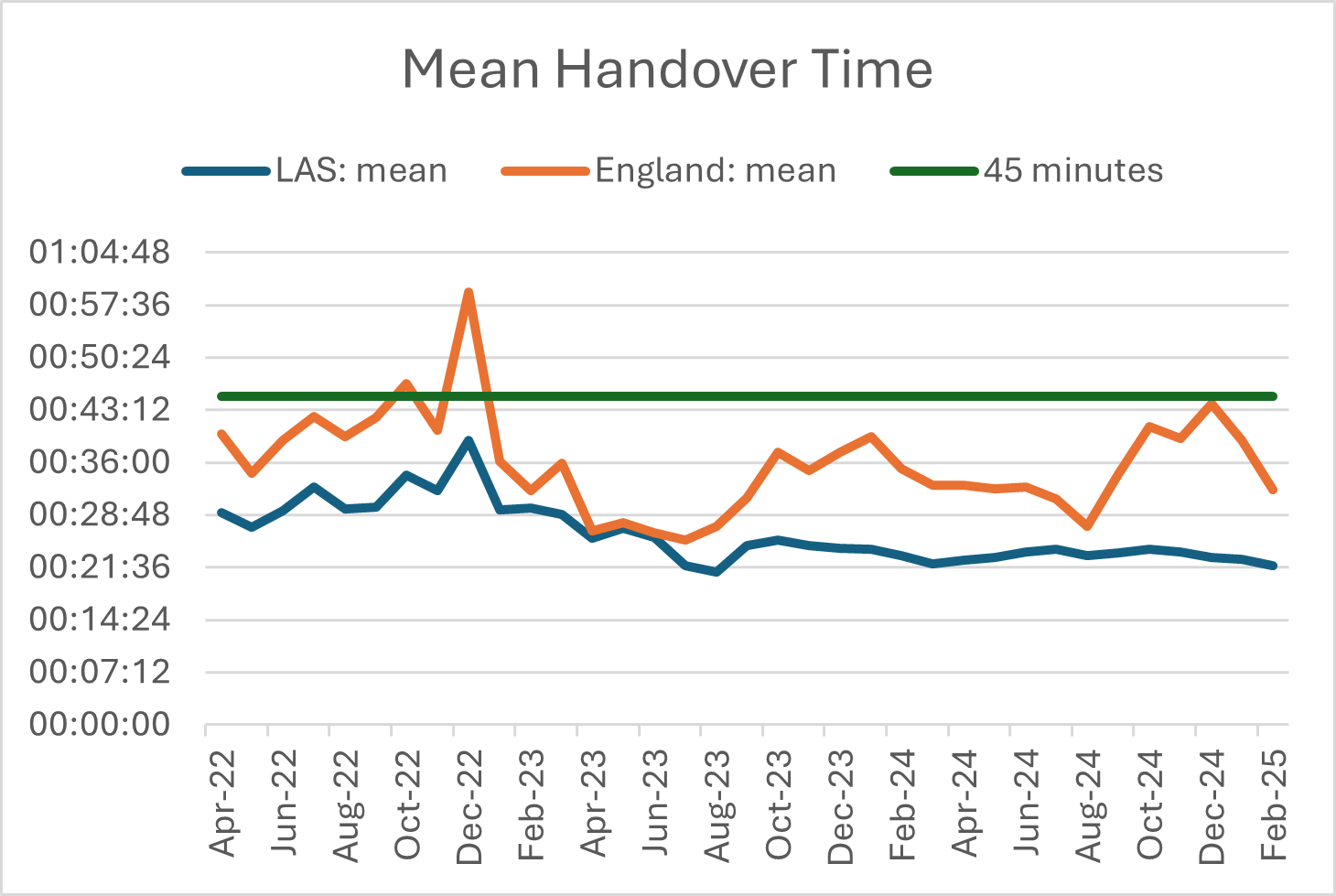
The national standards for hospital handover in 15 minutes and turnaround (time to crew availability) in 30 minutes still seem way out of reach. The NHSE priorities and operational planning guidance for 2025-26 stated that systems should implement. ‘…joint working arrangements that ensure that no handover takes longer than 45 minutes, working towards delivering handovers within 15 minutes.’ In March 2025 the mean handover time in England was 29 minutes 17 seconds, with 9% of all handovers taking longer than an hour.
Introducing the W45 (withdraw at 45 minutes) – or alternatively called ‘rapid release’ protocol – has proven more challenging for some hospitals than others. Investigations for a recent Health Service Journal article found that, ‘…of 30 hospitals who have yet to introduce this policy, seven were national outliers for the number and proportion of handovers taking more than an hour over winter.’
Unhelpful references to ‘drop and go’ or patients being ‘dumped’ in hospital corridors have made establishing such procedures even harder and, in some cases, have put an additional unfair strain on working relationships between ambulance and ED staff, all of whom are focussed on the safety of their patients in difficult circumstances.
Of course there are safety measures and criteria involved in escalating to W45 for each and every patient waiting in an ambulance. It is not simply the case that 45 minutes is up, and the patient is left in the ED without discussion. In most cases where a collaborative approach has been taken to introducing W45 we can see significant, and often immediate, improvements in handover times.
For some ambulance trusts, the concept of having an agreed maximum handover time of 45 minutes with all hospitals in their region has been in place for a number of years – for example SECAMB – and the outcome is clear with their mean handover times and percentage of hour-long delays being consistently well below the national averages, as these graphs illustrate:
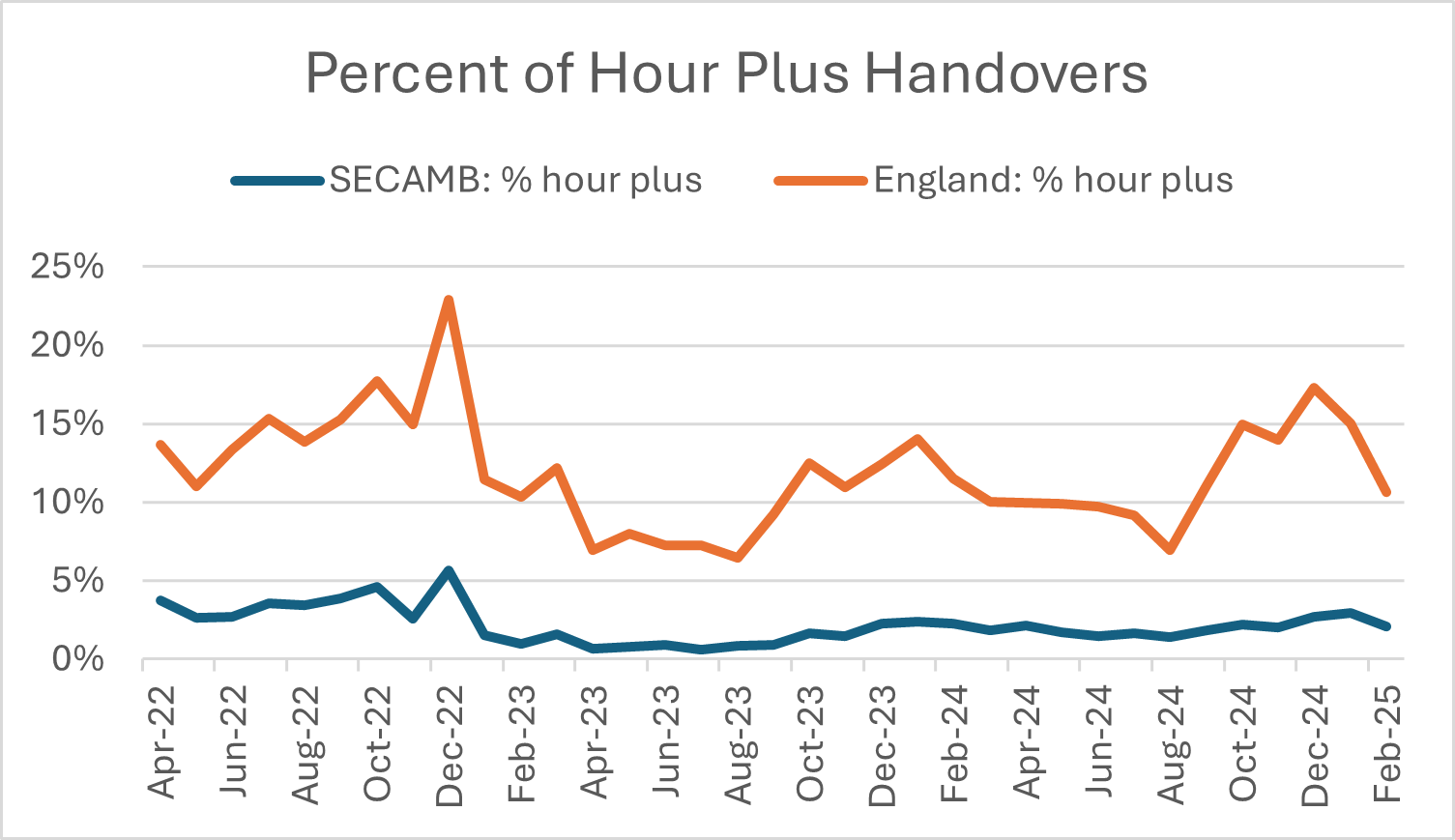

For others, such as LAS, who began gradually introducing W45 in the last couple of years with the London hospitals, the impact is more noticeable, particularly in the drop in percentage of hour plus delays from August 2023.
You can listen to staff describing how King George Hospital in London worked with LAS to introduce W45 in the Summer of 2023 and the positive impact this had not only for patients but also for the staff in both trusts.

Anna Parry, Managing Director of AACE, said in a recent statement:
Hospital handover delays continue to be a major issue affecting ambulance service performance and the quality of patient care, as they have been for several years now, something the data underlines heavily. However, we are starting to see positive improvements in areas where ambulance services have been able to work very closely with their colleagues in many hospitals to ensure faster but safe patient transfers from ambulance to emergency department care, often in under 45 minutes.
We know that to achieve consistently good quality care for patients receiving urgent and emergency care services, close collaboration between ambulance service employees and emergency department employees is imperative. However, it is also imperative that the key reasons for the bottlenecks being caused at hospitals are addressed nationally, especially delayed discharge of patients who are fit to go home and gaps in social care that prevent many from doing so.
Ambulance trusts in many parts of the country have moved towards a process where there is a maximum time allocated for a transfer of care from the ambulance service to the receiving hospital. This has in general – and where there has been close collaboration between ambulance and hospital trusts – proved to be a positive outcome for patients which is clearly something that AACE believes should be considered by all local health and care systems.
So in summary, there are good reasons to believe that the adoption of these rapid release protocols has led to lower handover delays and better experiences for patients and staff in many areas of the country.
The key for success in these initiatives clearly lies in a joint commitment to improving experiences for patients and staff, alongside positive, close working relationships between ambulance, hospital, ICB and other local health and care partners to make them work.